Videothoracoscopic (VATS) lobectomy, a minimally invasive technique, has been performed for approximately 20 years [1]. The advantages include improved patient satisfaction due to less surgical trauma, less postoperative pain, faster recovery, and less invasiveness compared to open surgical techniques [2]. Endoscopic vascular and parenchymal staplers are widely used for video-assisted thoracic surgery (VATS) and are mostly considered a safe technique [3].
In our case report, a patient, who underwent uniportal VATS lobectomy for lung adenocarcinoma and who was reoperated on due to the development of massive right internal mammary artery bleeding due to the intraoperative use of stapling, is presented.
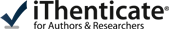
In the thoracic computed tomography of a 63-year-old female patient, a nodule with irregular margins was present in the inferior part of the upper lobe of the right lung. A transthoracic biopsy was taken from the nodule and the pathology result was reported as lung adenocarcinoma. The patient underwent right upper lobectomy and mediastinal lymph node dissection with uniportal VATS. Since the major and minor fissures were incomplete, they were intraoperatively separated with an endoscopic 60-4.8 parenchymal stapler. There was no decrease in hemoglobin value and no pathological finding on chest radiograph until postoperative day 4 (Figure 1). On postoperative day 4, the patient suddenly had hemorrhagic drainage. The patient had 500 ml of hemorrhagic drainage from the chest tube within 30 minutes. The patient was operated on in emergency conditions due to an appearance consistent with hematoma in the right hemithorax on chest radiograph (Figure 2) and decreased hemoglobin level. The uniportal VATS incision was extended posteriorly to provide access to the thorax. After the evacuation of approximately 1000 ml of hematoma, a bleeding focus was noted in the right internal mammary artery and was primarily sutured, and the bleeding was controlled. The bleeding originating from the internal mammary artery was thought to have occurred after the injury by the staple edge placed in the middle lobe to separate the minor fissure. The staple at the end was removed to prevent re-bleeding, and the area was sutured using 4-0 prolene suture. Intraoperatively, the patient received 4 units of erythrocyte suspension replacement. The hemoglobin value postoperatively reached a normal level. The patient’s postoperative chest radiographs showed expanded lungs with no pneumothorax or effusion. The patient with no pathological finding on the chest radiograph taken after the removal of the chest tube was discharged.
Figure 1
Preoperative posteroanterior chest radiograph and postoperative 4-day posteroanterior chest radiograph
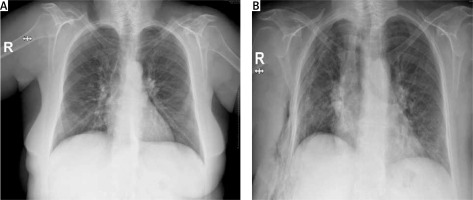
Figure 2
Posteroanterior chest radiograph taken on postoperative day 4 when the patient’s drainage started

The first uniportal VATS lobectomy was performed by Gonzalez-Rivas at Coruńa University Hospital [1]. Uniportal VATS is a less invasive approach that allows thoracic surgery operations carried out with large incisions to be performed with a single small incision of approximately 4 cm. The advantages include improved patient satisfaction due to less surgical trauma, less postoperative pain, faster recovery, and less invasiveness compared to conventional VATS [2]. Complications of the videothoracoscopic techniques are rare with an estimated frequency of approximately 3–4%. The most frequent complication is postoperative prolonged air leak. Other significant complications are bleeding, infections, and postoperative pain [4]. Surgical vascular and parenchymal staplers are widely used for VATS and are mostly considered a safe technique. However, late complications such as hemoptysis and intrapulmonary hematoma caused by stapled lung resection have been reported [5]. Although the use of stapling rarely causes serious complications, some articles have described staple-associated late hemothorax that requires an operation [5, 6].
Motoyama et al. reported that a patient who underwent right lower lobectomy with VATS for lung cancer developed hemothorax immediately after discharge. Operative findings suggested that bleeding resulted from the injury to the intercostal artery by staples used in the right lower lobe vein [5]. Sakaguchi et al. also reported a similar case of hemothorax with injury to the right intrathoracic artery caused by a staple [6]. Our patient was reoperated on due to the development of massive hemothorax on postoperative day 4. The intraoperative findings suggested that the staples used in the right middle lobe parenchyma injured the right internal mammary artery.
In conclusion, although the use of an endostapler in videothoracoscopic surgery is considered safe, it should be kept in mind that it can injure adjacent vascular structures and organs, resulting in fatal complications such as massive bleeding. In order to avoid staple-associated hemothorax, care should be taken to ensure that the staple line is smooth, and staples with open sharp ends should be removed.